Robotic Assisted Technology
RoboKnee is a sophisticated, patient-specific knee replacement program at USC Center for Hip and Knee Replacement (CHKR) in Los Angeles under the direction of Dr Andrew Yun. Patients are comprehensively treated with patient-specific surgery, patient-specific hospitalization, and a patient-specific recovery. Each phase of treatment is tailored to the individual’s anatomy, level of fitness, medical health, and social circumstances. Following the Rapid Recovery Protocols, many are walking comfortably within 3 hours of surgery and climbing stairs the same day. We offer the options of Same Day Discharge, Overnight or Extended Stays.
The Roboknee Program
Roboknee is based on the Mako Surgical Robotic System that leverages 3D modeling to minimize bone and tissue dissection. The Mako is a proven leader in robotic technology, and Saint John’s is validated among the highest performing robotic knee replacement programs in the country.
- Patient specific surgery: Know more and Cut less
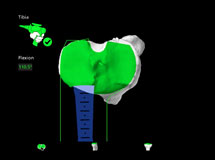
- Anatomic modeling based on 3-Dimensional CT scans for customized fit, sizing, and placement. Tall or short, wide or thin, male or female – all operative planning is analyzed and completed prior to surgery.
- Patient specific soft tissue balancing during surgery optimizes positioning and alignment to correct pre-existing deformities.
- To protect soft tissues Using robotic software, a virtual boundary is placed around the bone beyond which the instruments cannot cut.
- Muscle sparing techniques preserve the quadriceps tendon and hamstring function.
- Stryker Triathlon Total Knee Replacement and Restoris MCK Partial Knee Replacement have outstanding long term durability and performance in national registry data.
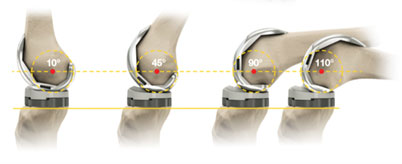
- Bone conserving design with a single radius of curvature for a natural range of motion
- Condylar stabilized bearing surfacing with PCL retention using highly cross linked polyethylene
- Fixed bearing design for rotational movement and stability.
- Antibiotic loaded cement fixation for long term durability and minimization of infection
- Mako Robotic Surgery platform
- The precise surgical technique is based on anatomic balancing preoperative bone planning with 3D modeling, real time ligament balancing to correct pre-existing deformities, and intraoperative fine tuning to establish a stable alignment and natural range of motion. Initially, a preoperative CT scan of the knee is converted into a virtual 3D model of the bone anatomy. Implant sizing, fit, alignment, rotation, and positioning are then defined with a measured resection philosophy based on bone conservation.
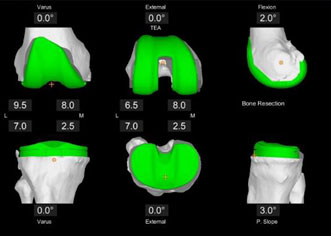
In surgery, the degrees of ligament deformity in the coronal and sagittal planes are then characterized and correlated with the anatomic bone model prior to bone preparation. Micro-adjustments are then made to optimize mechanical alignment, bone conservation, posterior condylar offset, implant rotation, joint line height, and patellar tracking. Trials of the actual implants are then used to verify flexion and extension gap balancing, range of motion, and correction of deformity using an 8 point checklist. - Every patient has unique medical and social needs. Rather than sending everyone home the same day, the RoboKnee program at Saint John’s stratifies a patient’s needs and wishes to offer three separate tracks.
- Same Day Surgery. Patients who are sufficiently healthy and supported will have the option of going home within hours after surgery once they have cleared medical and physical therapy goals.
- Overnight Stay. Patients with pre-existing conditions that require observation will be asked to stay overnight for monitoring. Patients who request additional therapy, nursing, or support will also have the option of an overnight stay.
- Extended Stay. Patients who require more aggressive medical or social support after surgery will have the option of a longer hospital stay or even transition to a skilled nursing facility. Hospital benefits of RoboKnee, applies to all three tracks.
- No blood transfusions. All surgeries performed with blood conservation protocols.
- No routine urinary catheter. Bladder ultrasounds are used to follow urine output.
- No routine blood draws
- No skin staples and all patient receive plastic surgery waterproof closure with absorbable stitches.
- Walking within hours of surgery
- Climbing stairs the same day
- Same day Physical Therapy
- No walker or crutches.
- PT comes to home for ongoing training.
- Outpatient therapy in your neighborhood
- Next day shower options.

- Pain Control
- Knee Replacement is a painful surgery, but organized pain management protocols make recovery far more manageable.
- Dedicated orthopedic anesthesia team. Spinal, regional or general anesthesia options available based on medical need and patient preference.
- Long acting periarticular blocks with local anesthetic injection in the knee
- Multimodal pain control – NSAIDS, steroids, nerve medications to minimize need for narcotics
- Customized pain management plans with pain management doctors and pharmacist teams available
- Extended release, On-Q system for up to 5 days of pain relief
- Patient specific education variety of patient educations options depending on individual needs and preference.
- Knee replacement is a major surgery. Surgery always carries risks. Recovery is physically strenuous and emotionally challenging. Facing the need to have knee replacement can be frightening, but preparation and information ease the anxiety.
- Each patient receives a notebook to be used as a detailed roadmap for preparation, surgery, and recovery.
- Live classes on knee replacement are held in the orthopedic wing of the hospital for preoperative training, physical therapy, and nursing.
- Alternative online Zoom classes for small group virtual teaching and preparation or, individual zoom session available
- Technical specifications:

Patient specific Hospitalization
Patient specific Recovery
Physical Therapy

Frequently Asked Questions
Background
But What is Arthritis, and What is a Knee Replacement?
In a healthy knee, there is a thick layer of cartilage that lines the ends of the bones and allows for smooth gliding motion as well as knee stability. Arthritis is a progressive degenerative condition whereby the cartilage wears away and becomes ragged. As a result, the exposed bone ends rub together creating pain, instability, and deformity. Patients often notice they have become “bow-legged” or “knock-kneed” over time. They may also notice an inability to fully straighten or bend the knee. Sometimes, the knee will buckle and collapse. These are all manifestations of arthritis.
The objective of knee replacement surgery is to restore smooth surfaces to the ends of the bones and replace the lost cushion such that the knee regains a smooth and full range of motion, anatomic alignment, and stability.
Dispelling the Myth—Replacement or Resurfacing?
Many people have a vague idea of knee replacement that often involves cutting the bones above and below the knee, and replacing the knee joint with a contraption that mimics a knee. That couldn’t be further from the truth. Modern knee replacement is more accurately described as a knee resurfacing procedure. The worn cartilage and uneven bony surfaces of the femur, tibia, and patella are reshaped, smoothed out, and capped by metal and polyethylene caps. There are many different manufacturers of knee replacement implants, many surgical approaches, and a wide variety of surgical instrumentation that can be used to accomplish this.
Minimally Invasive?
Despite being a resurfacing procedure, it is important to understand that knee replacement is still major surgery. Over time, evolving approaches and more advanced instruments have allowed surgical incisions to become shorter and soft tissues to be more protected, but they have not transformed a major surgery into a “minimally invasive” one. The joint still needs to be exposed to some degree in order to resurface the bones and secure the caps. Any surgery will result in post-operative inflammation characterized by pain, swelling, and stiffness, and knee replacement is no different.
However, major advances in operating room technology, pain management, and rehabilitation have made surgery and recovery far less physically and emotionally traumatic.
Our Team

Andrew Yun, M.D.
Director
As a board-certified orthopedic surgeon, he is a nationally recognized specialist in hip and knee joint replacement, specializing in anterior hip approach, robotic total and partial knee.
www.TotalJoints.net